Think of a traditional European meal. First, you’d have starters, maybe a soup, then your main dish, usually something with meat, then you might have dessert, or cheese – or even both! And, depending on what you’re eating, you might be advised to pair it with different wines, or ale. Of course, how people eat varies widely across time and …
Green Sickness and Virginity
From the mid-16th century to the early 20th century, young girls described as suffering from bodily weakness, dietary disorders, heart palpitations, fainting spells, paleness, and an absence of menstruation (amenorrhoea), were often given the diagnosis of ‘green sickness’, the ‘disease of virgins’.
What is the Humoral Theory?
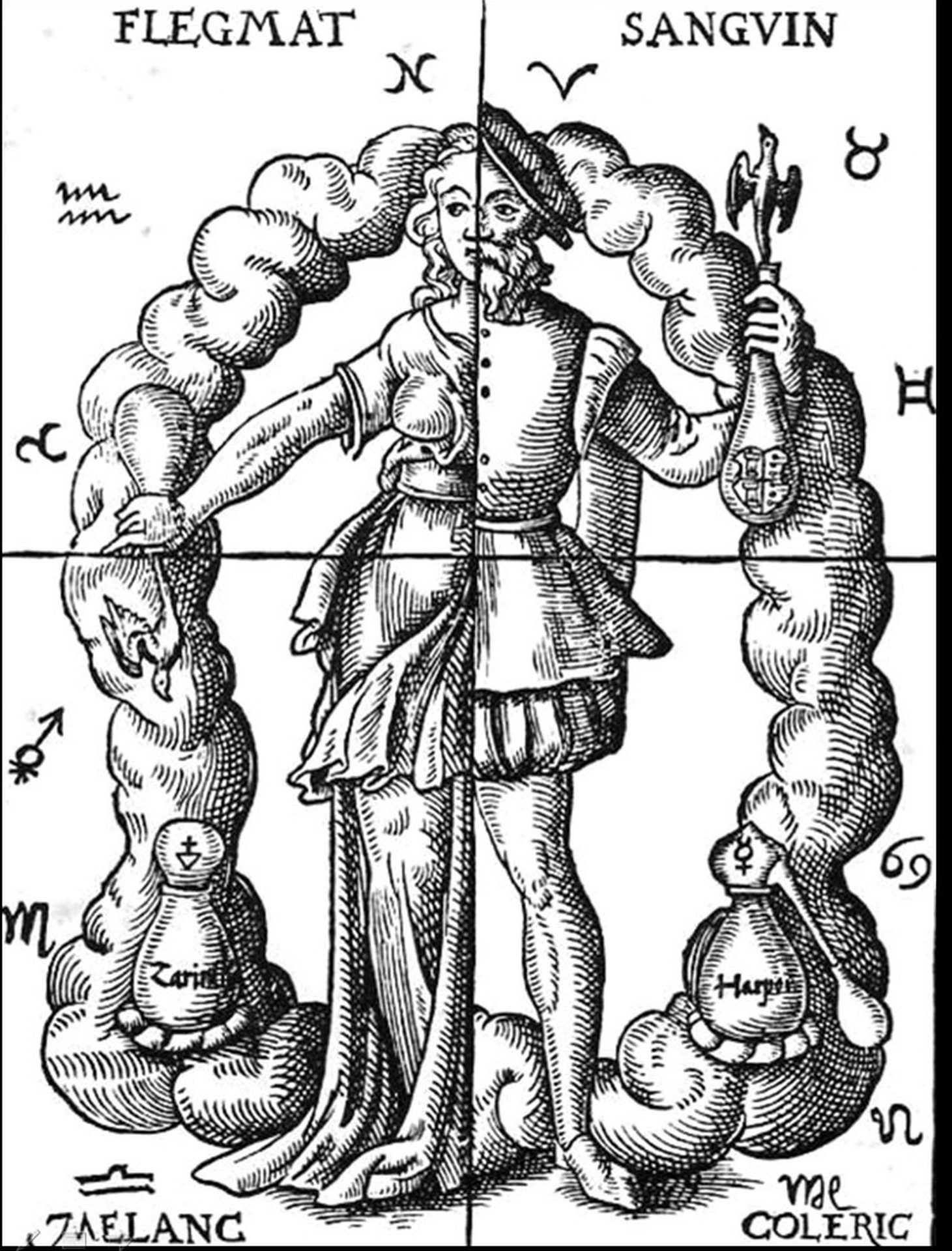
Humours are everywhere. People can react cholerically to an insult, music can make us melancholic, time with friends can lift our spirits, and we can be in good or bad humour. This is not surprising. The humoral theory has a long history, beginning with the Greek Hippocratic writers in the fifth century BC, being reinterpreted by the Roman physician Galen in the second century AD.